Originally published to Becker’s Hospital Review
In October of 1918, during the height of the Spanish Flu pandemic, citizens of Philadelphia held a parade with a marching band and Boy Scouts in uniform, despite protests from the scientific community.
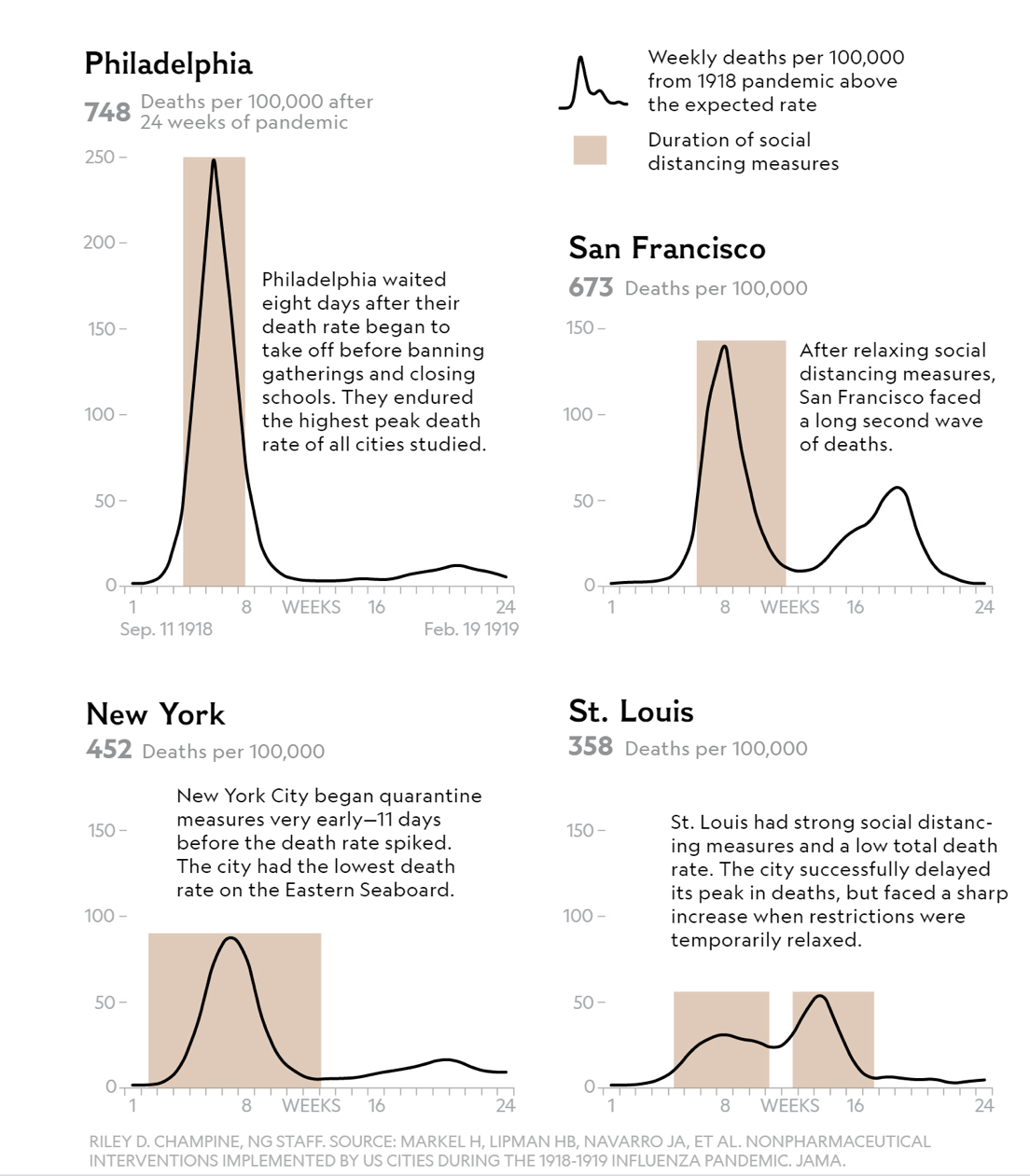
As a result of Philadelphians’ disregard of social distancing directives, 837 people died in a single day; 4,500 in a week; 17,500 within six months. In New York City and San Francisco, citizens listened to the scientific community and put in place stay-at-home orders. San Francisco subsequently relaxed its orders resulting in a second peak. Most interestingly, St. Louis put in place early strict stay-at-home orders, but the Spanish Flu had a second, larger peak when orders were subsequently relaxed (Shown in Figure 1). History tells us that what we do matters.
Figure 1: Lessons from the Spanish Flu via National Geographic
The lessons learned from the Spanish Flu pandemic provide a good starting place for a conversation on COVID-19, but that historical experience does not tell the entire story. COVID-19 is distinct from any other modern pandemic because its impact on the U.S. will be greater than any health related crisis in a hundred years. Much has been written about COVID-19, but this three-part series will focus on the short and long-term impact upon hospitals and the innovation and transformation needed to survive. Part I will discuss the health care implications of the disease: its potential duration, magnitude, and the ‘new normal’ for hospitals. Part II will focus on the significant impact on hospital finances and broader economic implications. Finally, in Part III, the focus will be on the response and how hospitals must transform to deliver sustainable clinical care for their COVID and non-COVID patients in order to maintain economic viability.
Hospitals Should Expect at Least Two Years of Disruption
Many experts are trying to figure out exactly how long COVID-19 and its disruption will last. Leading experts at Johns Hopkins, The Gates Foundation, and others have extensively researched the virus and its possible scenarios. Our team of health professionals and data scientists at Neeka Health Intelligence have been working diligently with our partners for the past three months to create an early multiparametric scenario modeling tool that has now been validated by multiple resources. Our tool demonstrates various scenarios based on a series of input variables: social Isolation (i.e., duration and magnitude), impact of the disease (i.e., hospitalizations, acute care, and mortality rates), availability and impact of therapeutics and vaccines, and, testing parameters (i.e., sensitivity and specificity).
In the model below (Figures 2 and 3) we illustrate high and low impact scenarios. In both simulations illustrated below the input parameters are:
• Mortality rate (1%)
• Acute care rate (1.2%)
• Hospitalization rates (2.4%)
• Vaccine availability in April 2021
In the high and low scenarios shown, the only difference being in the first scenario (Figure 2) strict social isolation is continued through December 1, 2020. That date, which is economically intolerable, does result in a relatively negligible second peak. In the second scenario (Figure 3) we show a currently proposed recommendation, with relaxation of stay-at-home orders scheduled for June 1, 2020. Unfortunately, the trade-off for economic benefit in the latter scenario may be a second (much larger) peak. However, the model is granular enough to consider geographic variance based on the initial local and regional efforts.
Figure 2: Scenario analysis for New York State, assuming strict stay-at-home orders until December 1, 2020
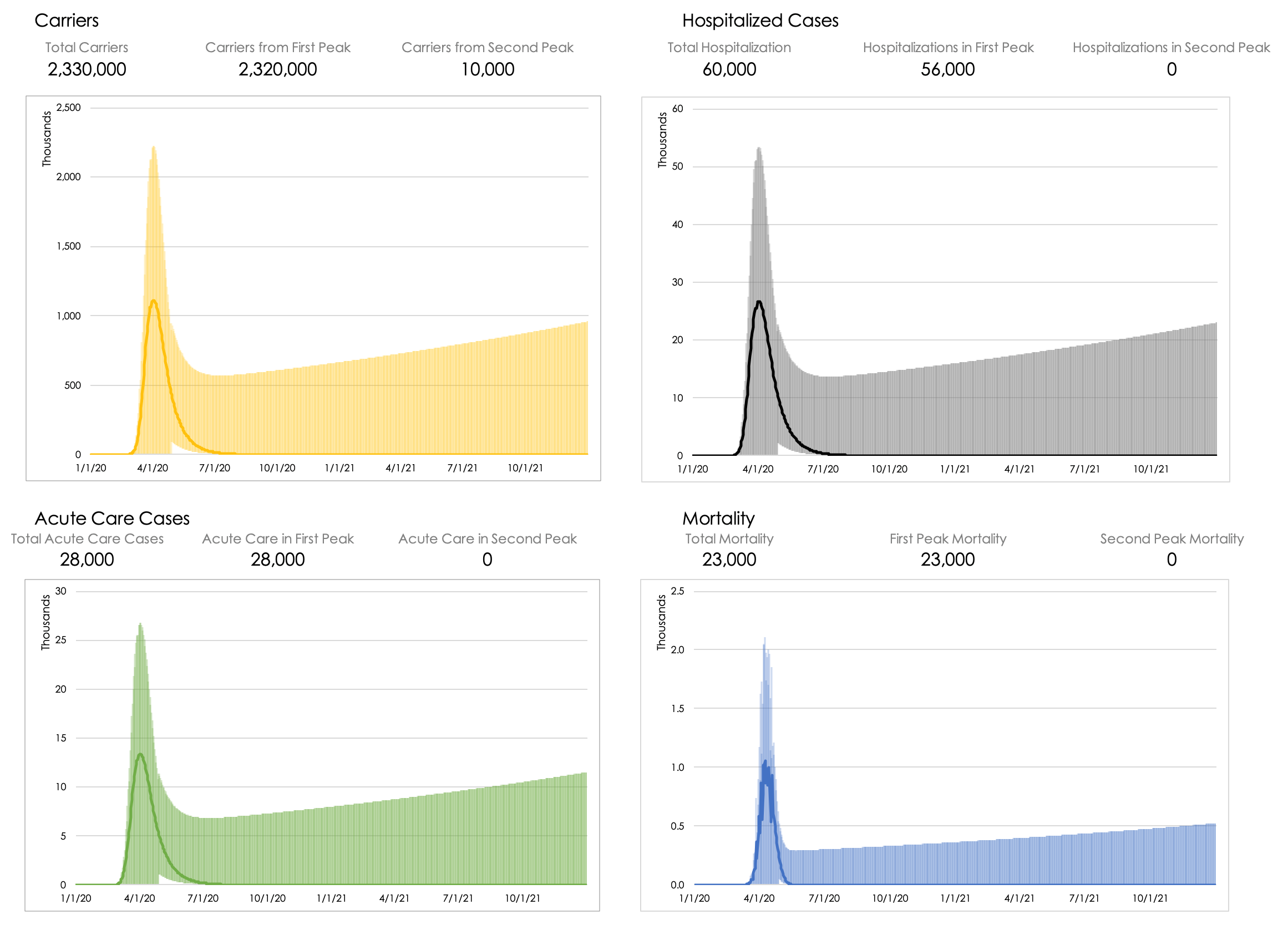
Figure 3: Scenario analysis for New York State, assuming stay-at-home orders until June 1, 2020 (and no second wave restrictions)
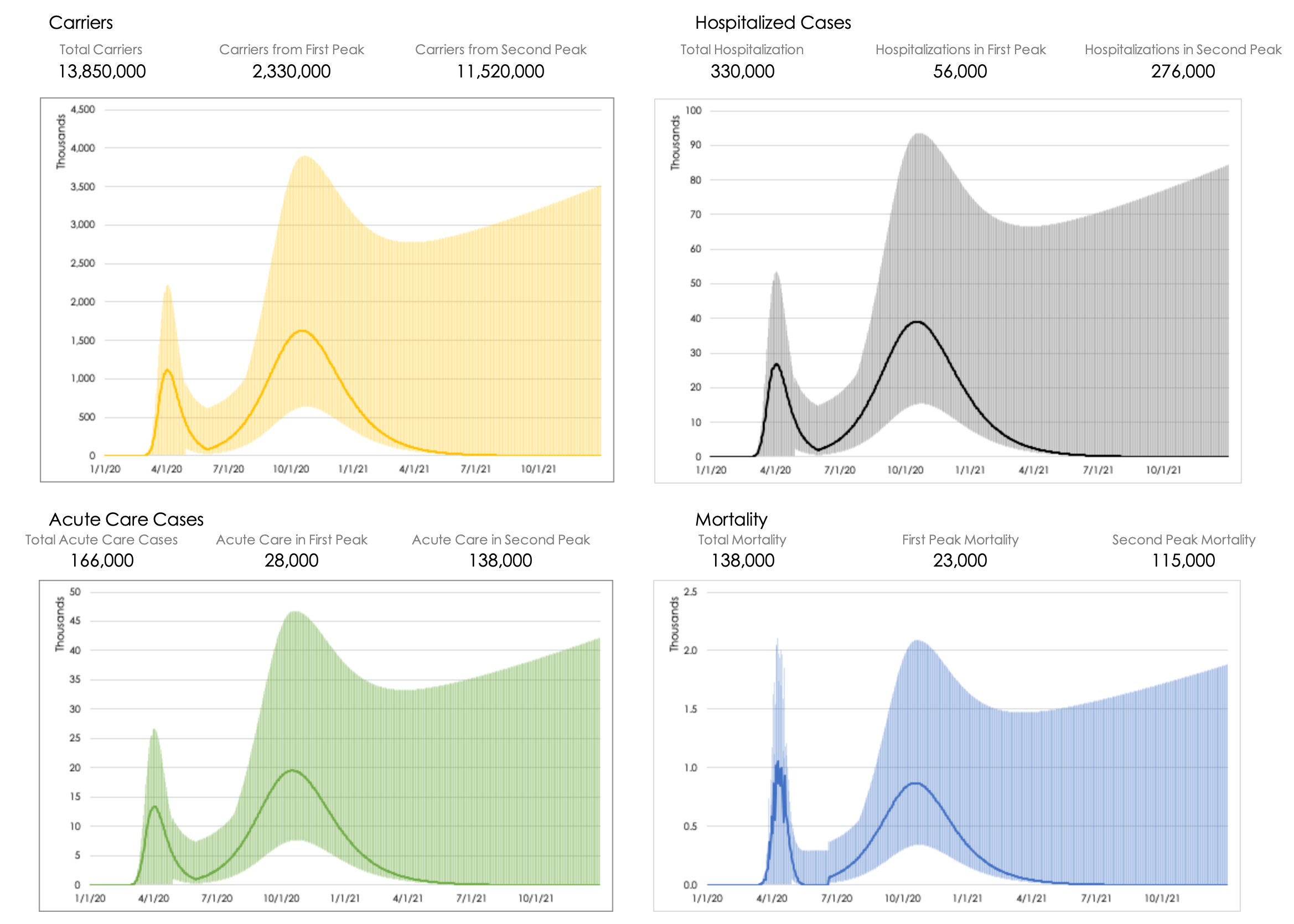
In these examples, we demonstrate an unlikely scenario (December 1st) and a more likely scenario (June 1st) based on current socioeconomic and political factors. Consistent with the lessons learned from Spanish Flu, it is clear that our initial response to COVID-19 and when we relax stay-at-home orders may determine the severity of a second or third peak. Unless data-driven policies are put in place, there may be more hospitalizations and acute care needs, which threaten to exceed the capacity of our already strained health care system.
Background on COVID-19
Compared to past infections that had the potential to become pandemics, COVID-19 is unique. Typically, pandemics are very infectious and have a high mortality rate compared to more common seasonal illnesses. Like prior pandemics, COVID-19 is highly infectious and has a high mortality rate compared to seasonal influenza. However, COVID-19 is unique because of its combination of being highly infectious and, despite having a relatively high mortality rate, the rate is low-enough to allow the disease to circulate through the remainder of the population without ‘burning itself out’.
The results of COVID-19’s unique nature is a greater overall mortality as it infects a larger portion of the total population. COVID-19 is, essentially, a slow but effective silent killer; rather than the explosive and relatively quick impact of Ebola. As well, by virtue of its insidiousness, COVID-19 is resource intensive for healthcare providers as it often leads to prolonged hospital stays (up to weeks) leading to high economic burdens.
Contagiousness
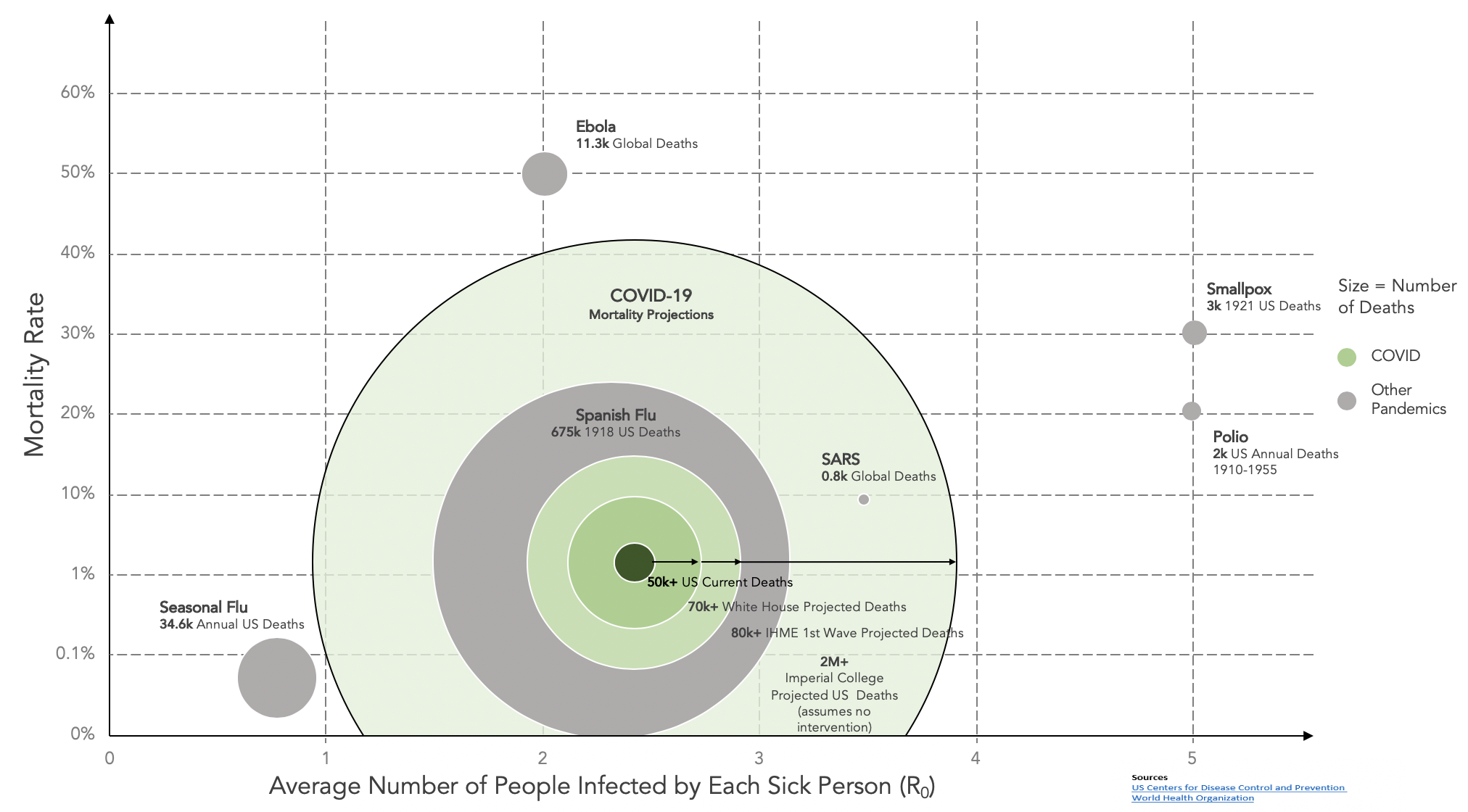
The Centers for Disease Control (CDC) and World Health Organization (WHO) use R0 to indicate the basic transmissibility rate of an infectious agent. Many diseases have a high R0. For instance, smallpox has an R0 of 3.5-6, which means every sick person, on average, infects approximately three to six others. Other common infectious diseases, such as the seasonal flu, infect on average less than 1 person per infected person. Ebola had an R0 of 1.5-1.9 and SARS an R0 of 2-5.
COVID-19 has an R0 between 2.2 and 5.7. The range is quite wide given the limited understanding of transmission factors as well as the difficulties of global reporting of data. Its R0 is most closely aligned with Polio or Smallpox. Suffice to say it is more transmissible than its pandemic cousin, the Spanish Flu. Relative R0 and mortality rates are illustrated for the major pandemics in Figure 4. For more on this topic, please read the Gates Notes.
Mortality
COVID-19 is not as deadly as some diseases – e.g., Ebola, Polio, and Smallpox – but is almost certainly more deadly than the seasonal flu. Again, due to poor testing information in the U.S., the exact mortality rate is unclear, but other countries are providing guidance on the expected ranges. For instance, note the following results:
• South Korea – 2.2% fatality rate (10,718 confirmed cases vs 240 deaths)
• Germany – 3.75% fatality rate (155,788 confirmed cases vs 5,835 deaths)
• Iceland – 0.56% fatality rate (1,790 confirmed cases vs. 10 deaths)
Considering the Spanish Flu mortality rate was ~1% per infected people, it is likely COVID-19 is at least as lethal.
Figure 4 Magnitude and Contagiousness of COVID-19 Compared to Other Diseases
Duration
What is more insidious about COVID-19 is that it does not kill its host quickly. COVID-19 can take 1-2 weeks to show symptoms and can present asymptomatically or with very mild symptoms in a large portion of the population, which increases the transmission opportunities. For those who have acute symptoms, the disease can take upwards of 20 days to kill the host. Even if the patient recovers, they are in the hospital (all too often in an intensive care bed) for a few weeks. This leads to significant strain on hospital resources and requires challenging resource allocation decisions for doctors. The economic impact of long patient stays combined with high intensity care has a significant impact on a hospital’s operating margin, which (pre-COVID-19) was already razor thin.
Bottom line: Given the high infection rate, relatively high mortality rate, and long disease duration COVID-19 has the potential to persist within a population for a protracted time period.
Disease Response
As our team has modeled various scenarios, we have identified a substantial risk of a second (larger) peak if policy makers pursue early relaxation (as is already happening). There are only three potential tools to combat the virus: social distancing, therapeutic antiviral drugs, and immunization (i.e., vaccines).
Currently, we have only one tool available: social distancing. Social distancing can be strict or partial; the challenge with partial is that, given COVID-19’s infection rates (R0 = 2.2 and 5.7), if even a small number of people are infected and circulate in the general population they will spread the disease rapidly. While rapid disease spread may be desirable from a ‘herd immunity’ perspective, the relatively high-mortality rate (compared to seasonal influenza) may lead to an unacceptable toll on human life. We are witnessing the effects of limited social isolation in Sweden, which has ten times the number of deaths compared to neighboring Norway and Finland. Additionally, the hospitalization and acute care needs associated with subsequent waves may overwhelm the national health care system’s capacity.
The two other potential tools are therapeutics and immunization. Therapeutics are evolving and will require testing to prove efficacy. When an effective therapeutic is found, it will likely reduce severity of the disease, as with Remdesivir, but it will not durably solve the pandemic because it will not create herd immunity. Again, the Gates Notes nicely describes some of these therapeutics.
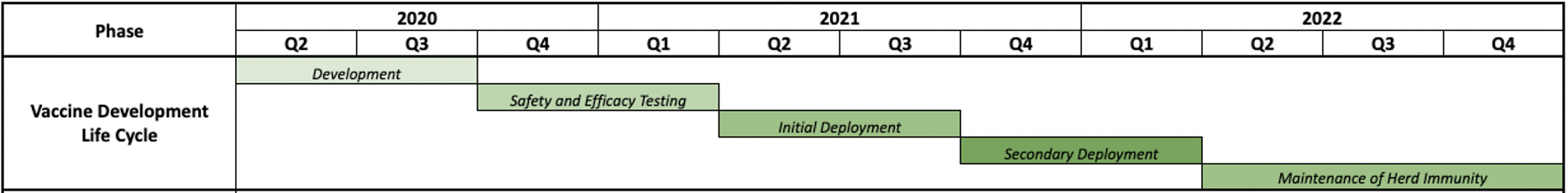
The other potential tool to combat COVID-19 is a vaccine. Under standard conditions, vaccines typically take 10 – 15 years to create so even in the most optimistic scenarios an effective vaccine will take 12 – 18 months to be developed, tested, approved, manufactured, and administered. We believe the process of vaccine development, safety and efficacy testing, and wide deployment optimistically will take 8 quarters (shown in Figure 5). If you compare the rate of transmission of COVID-19 carriers in the U.S. against the expected vaccine development timeline, without prolonged social distancing, much of the population will be infected before a vaccine is widely deployed.
Figure 5: Projected Optimistic Vaccine Deployment Timeline
The New Normal for Hospitals: The Next Eight Quarters and Beyond
All of this means that strict social distancing is currently our best available tool to control the spread of the virus. However, it is clear that economic realities will require social distancing compromises. While this may be construed as a necessity, we must do so with eyes wide open. Therefore, we should plan to manage the resulting surges as well as ongoing non-COVID patient care needs. All of this will culminate in a ‘new normal’ until an effective vaccine has been administered. During the new normal period, hospitals will continue dealing with or will be preparing to manage COVID-19 surges until the vaccine is adequately deployed.
This will create an unprecedented clinical and economic capacity strain. Hospitals will need to create patient strategies for both COVID-19 and non-COVID-19 patients. They will deploy considerable resources to flex staff. In order to be prepared for surges, hospitals may need to maintain partial (<70%) occupancies and 30-day supplies of personal protective equipment, further adding to fiscal strain. In geographies where COVID-19 cases spikes, exceeding capacity, doctors may be asked to make difficult decisions where all patients’ needs cannot be met simultaneously.
One compounding factor will be testing for COVID-19. As Dr. Michael Osterholm has noted, we do not currently have enough tests and some have limited effectiveness. Researchers found 15% of tests administered at the Cleveland Clinic produced false negatives. The implications of this false negative rate, given the R0, are chilling. Contact tracing is labor intensive, particularly during a peak, because the mechanics of tracing 2,000 new cases daily stretches the imagination. If issues related to testing persist, hospitals will need to utilize even more resources to identify and quarantine potential COVID-19 patients or, more likely, non-COVID-19 patients will avoid hospitals all together if they have the choice.
Testing could be further confounded by multiple factors. Including the following considerations:
• Availability of rapid point-of-care testing required for triage
• Absence of data to establish true immunity based on serology positive and antibody testing
• The possibility of positive patients being re-infected
• Scaling of testing
• If we could test a million people a day, it would take almost a year to test the entire U.S. population
• The possibility of effectively isolating positive patients
There are a significant number of testing research studies and conversations happening right now and the space is rapidly evolving.
Despite having to deal with COVID-19 patients for the next two years, hospitals still need to perform other procedures and provide other services. The strain on capacity and limited resources may put hospitals in an unenviable position where they are unable or unwilling to treat everyone due to risk of infection or resource constraint.
The Centers for Medicare and Medicaid Services (CMS) has provided guidance on how hospitals should prioritize patients. During the current peak they have been clear: hospitals still need to treat patients requiring urgent care – prioritizing strokes, brain bleeds, tumors, cardiac conditions, and cancer. These patients continue to present to emergency rooms, and, in fact, there is a backlog of cancer and transplant patients awaiting procedures. A second or third wave of COVID-19 will see a resurgence of urgent care, meaning longer waits in the emergency department. Unfortunately, some of these emergent conditions represent an unfavorable payer mix but should be cared for without question. The net result is further economic impact for health care systems and downward pressure on operating margins.
While expenses may increase or (at best) remain unchanged, revenues are at significant risk from the resulting loss of elective surgeries with a second wave of COVID-19. Additionally, some high margin inpatient procedures (e.g., surgical spine services) may permanently migrate to lower margin outpatient services. Ultimately, compelled by the forces of COVID-19 to delay high margin and elective procedures, hospitals will be under intense financial pressures struggling to look after their COVID-19 and urgent non-COVID-19 patients.
Under the new normal, patients will experience increased delays and wait times for services. Physical restrictions will reduce total amount of traffic through a hospital thereby relying increasingly on telemedicine. This will further affect hospital financials. Overworked and overstretched care providers may be subject to burn-out. Hospitals will face human resource challenges, turnovers, recruitment barriers and have to manage the spiraling morale effects of furloughs and layoffs.
Conclusion
COVID-19 will impact the U.S. healthcare system for two years. It will force hospitals to reimagine how health care is delivered. We should embrace the challenge. American ingenuity and resolve will lead the path forward. The solutions will require a new level of innovation and transformation of every facet of the science, integrated service delivery, and economics of health care.
In Part II of our series, we will explore the financial implications of COVID-19 and the needed innovation and transformation to ensure service continuity and economic viability. Stay with us and stay healthy.
About the Author: Dr. Kassam is a pioneering neurosurgeon, entrepreneur, and healthcare economic transformation thought leader. He has led four separate neurosurgical programs, each of which delivered innovative patient care with improved patient and financial outcomes. Dr. Kassam has a unique and proven patient-centric model for delivering financially-sustainable healthcare programs.
Neeka Health, LLC. Note: All charts are subject to uncertainties associated with any modeling assumptions and not intended for financial and health care treatment guidance.
